In the ever-evolving landscape of healthcare, the discipline of pharmacoeconomics has emerged as a vital tool for maximizing the value of healthcare resources and optimizing patient outcomes. Pharmacoeconomics, often referred to as the study of the economic and clinical outcomes of pharmaceutical products and services, plays a pivotal role in informing healthcare decision-making, resource allocation, and policy development. In this blog post, we’ll explore the importance of pharmacoeconomics in healthcare and its impact on patient care, healthcare systems, and society as a whole.
At its core, pharmacoeconomics seeks to answer fundamental questions about the value of healthcare interventions, particularly pharmaceuticals, in relation to their costs and benefits. By evaluating the costs and outcomes associated with different treatment options, pharmacoeconomic analyses provide valuable insights into the relative efficiency and effectiveness of various healthcare interventions. This information is essential for healthcare decision-makers, including policymakers, healthcare providers, insurers, and patients, as they navigate complex treatment decisions in an era of limited resources and escalating healthcare costs.
One of the primary benefits of pharmacoeconomics is its ability to inform rational and evidence-based decision-making in healthcare. By quantifying the costs and benefits of different treatment options, pharmacoeconomic analyses help stakeholders weigh the trade-offs and make informed choices about resource allocation, formulary management, and reimbursement policies. This enables healthcare systems to prioritize interventions that offer the greatest value in terms of improving patient outcomes and maximizing the efficient use of limited resources.
Moreover, pharmacoeconomics plays a crucial role in promoting cost-effective and sustainable healthcare delivery models. As healthcare costs continue to rise, payers and policymakers are under increasing pressure to contain costs while maintaining or improving the quality of care. Pharmacoeconomic analyses provide valuable insights into the cost-effectiveness of different interventions, allowing stakeholders to identify opportunities for cost savings, waste reduction, and efficiency improvements within the healthcare system.
Additionally, pharmacoeconomics contributes to the development of evidence-based clinical practice guidelines and treatment protocols. By synthesizing and interpreting available evidence on the economic and clinical outcomes of healthcare interventions, pharmacoeconomic analyses help inform clinical decision-making and standardize best practices across healthcare settings. This ensures that patients receive high-quality, evidence-based care that is both clinically effective and economically sustainable.
Furthermore, pharmacoeconomics plays a critical role in facilitating access to essential medications and healthcare services, particularly in resource-constrained settings. By demonstrating the value of pharmaceutical products and services in terms of their impact on patient outcomes and healthcare costs, pharmacoeconomic analyses help justify investments in healthcare infrastructure, drug development, and access programs. This is particularly important for ensuring equitable access to life-saving medications and reducing disparities in healthcare access and outcomes.
In conclusion, pharmacoeconomics is an indispensable tool for maximizing the value of healthcare resources, optimizing patient outcomes, and promoting sustainable healthcare delivery models. By evaluating the economic and clinical outcomes of pharmaceutical products and services, pharmacoeconomic analyses provide stakeholders with valuable insights into the relative efficiency and effectiveness of different treatment options. Investing in pharmacoeconomics research and expertise is essential for driving evidence-based decision-making, improving healthcare quality and efficiency, and ultimately enhancing patient care and outcomes. As we continue to navigate the complexities of the healthcare landscape, pharmacoeconomics will undoubtedly play an increasingly important role in shaping the future of healthcare delivery and policy.
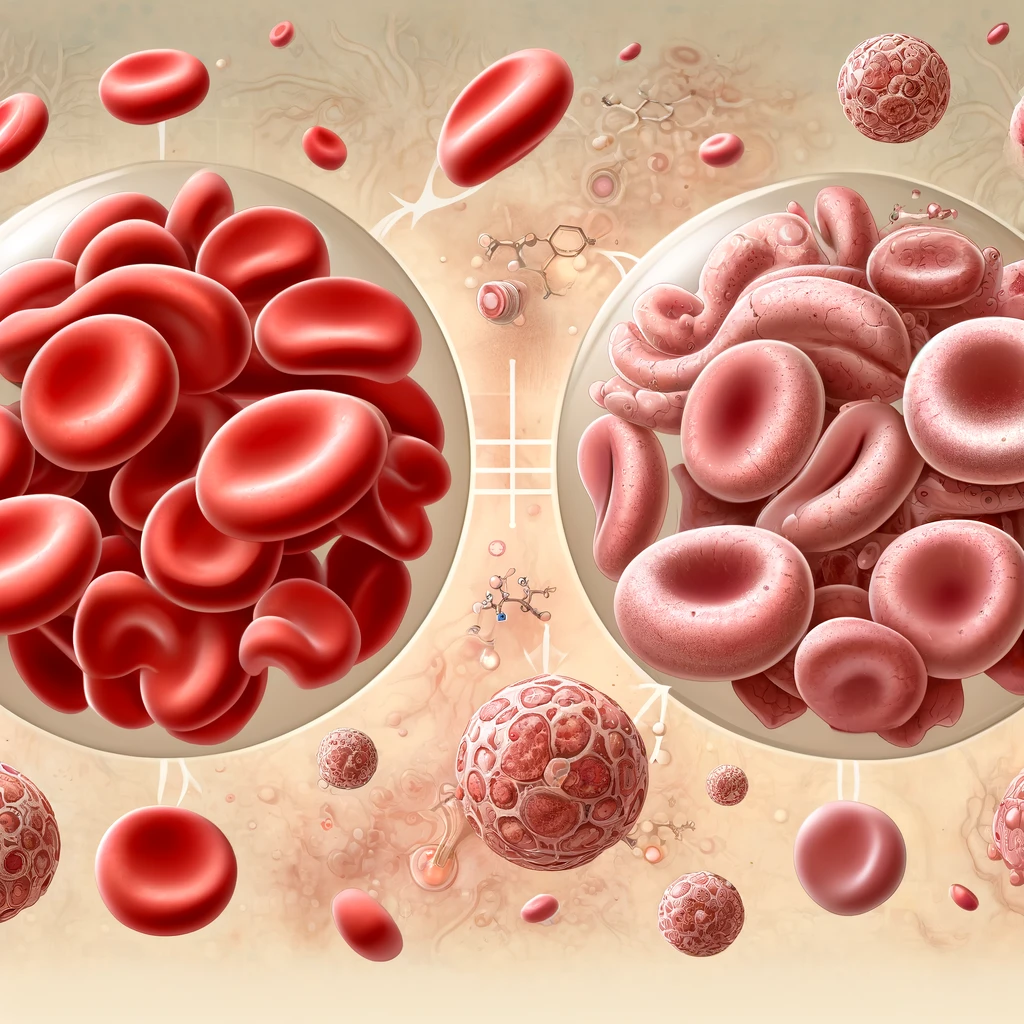
Iron Deficiency and Iron Deficiency related anemia contributes to several diseases worldwide. In 2016, more than 1.2 billion cases of iron deficiency anemia were reported. Iron deficiency anemia affects children, women in pre-menopause and people in low and middle income countries more.
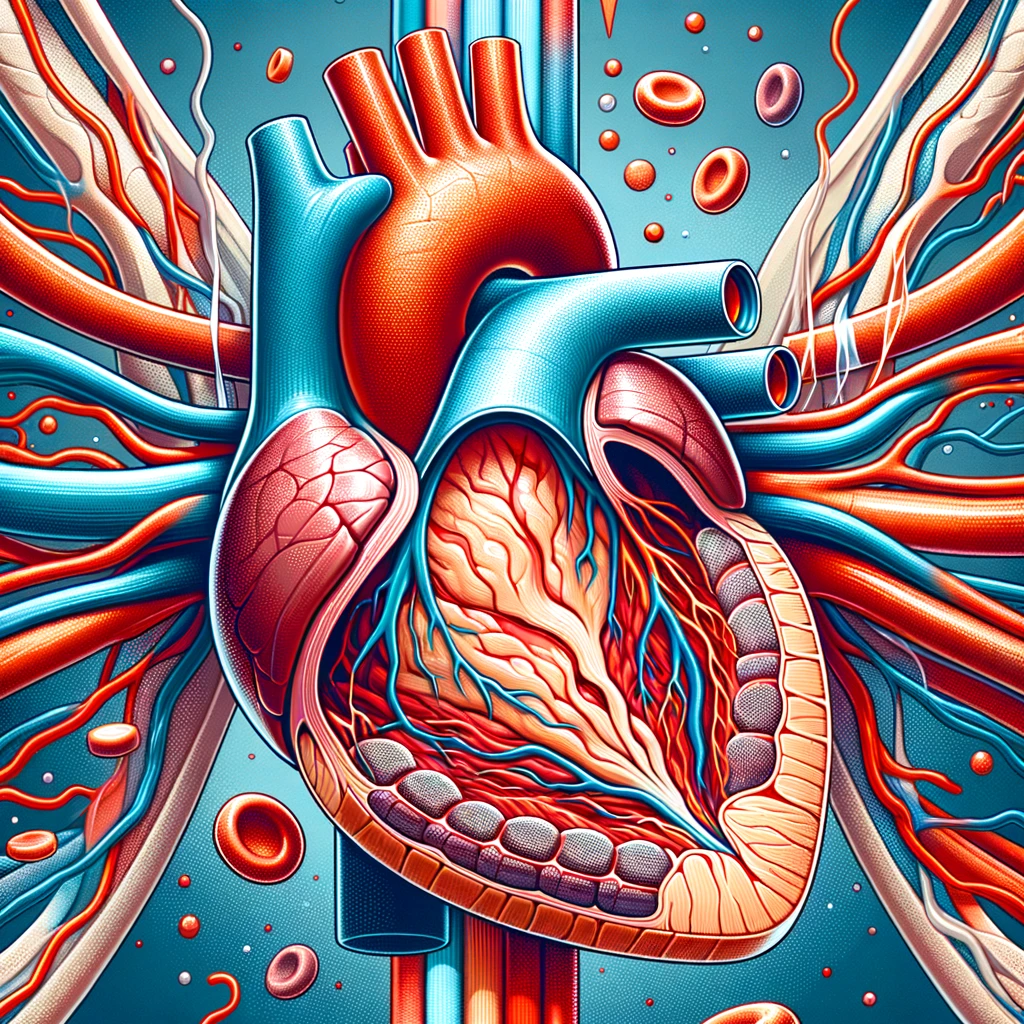
Myocardial infarction or acute myocardial infarction are the other terms for heart attack. The heart attack occurs when the blood supply to some certain areas to heart is disrupted and the heart muscle lacks oxygen and therefore gets damaged. In coronary arteries, which supply the heart, sometimes an obstruction may also occur. What this means is that an unstable plaque that consists of fat, cholesterol and white blood cells is formed and obstruct the vessel.
In the realm of healthcare, effective communication is paramount, especially when it comes to ensuring therapeutic safety for patients.
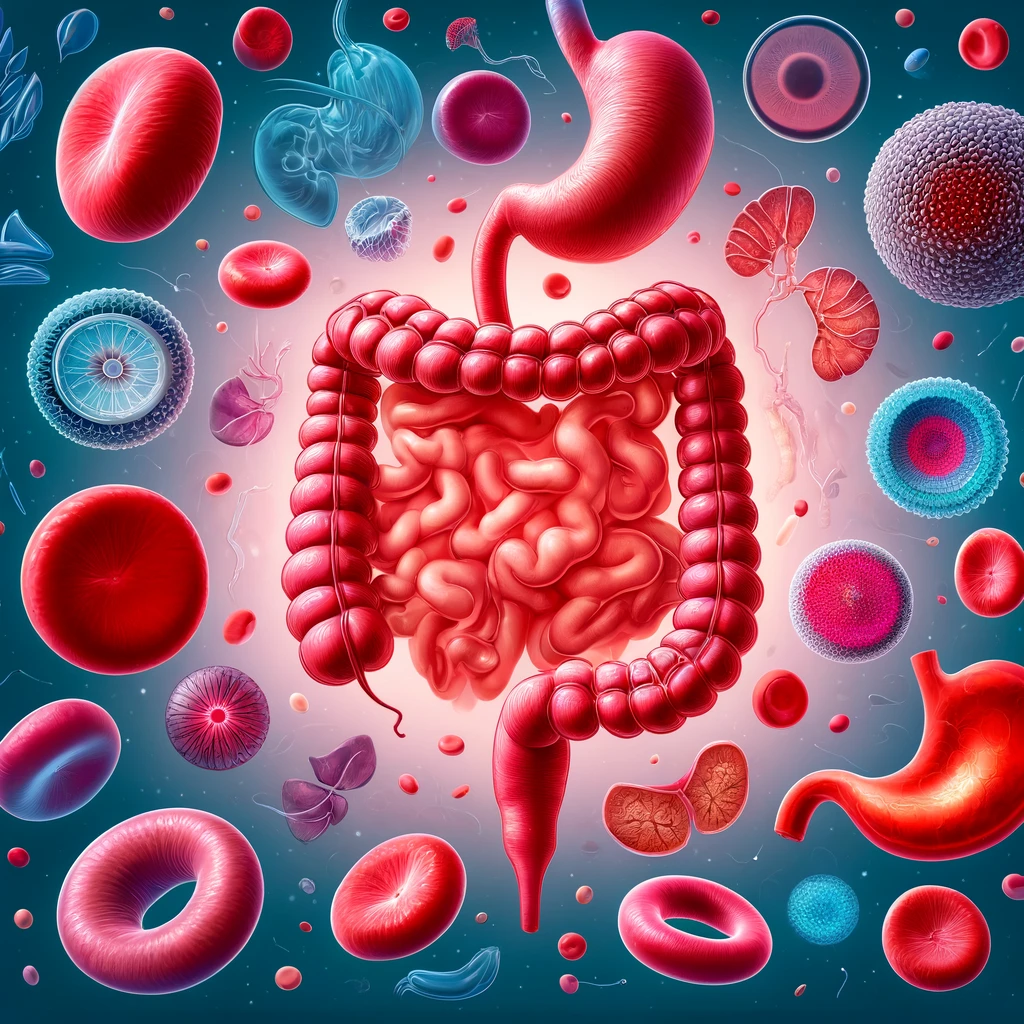
Once the Vitamin B12 is absorbed, it plays a key role as a cofactor in the synthesis of DNA, fatty acids or myelin. Therefore, Vitamin B12 deficiency could lead to both hematologic and neurologic symptoms.