Iron Deficiency
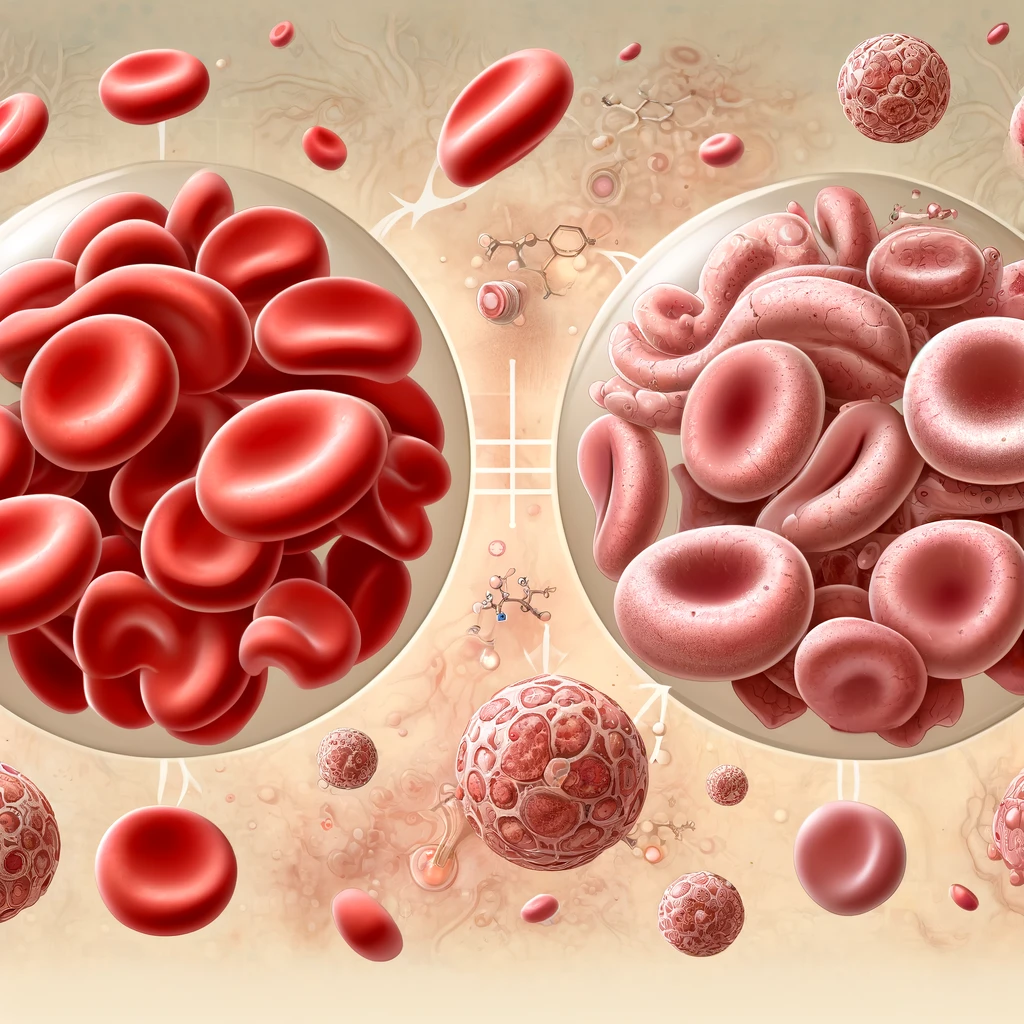
Iron Deficiency and Iron Deficiency related anemia contributes to several diseases worldwide. In 2016, more than 1.2 billion cases of iron deficiency anemia were reported. Iron deficiency anemia affects children, women in pre-menopause and people in low and middle income countries more.
Controlling the iron deficiency globally is in the priority list of World Health Organization, which aims to reduce the prevalence of anemia by 50% in 2025.
When the iron intake is not enough or lower than the body needs for itself, a compensation mechanism tries to prevent this physiological and pathological loss by using its own iron deposits. Absolute iron deficiency stems from when this compensation mechanism is not adequate for the body. This condition is common in children and women in pre-menopause especially who are pregnant.
Iron deficiency can either be symptomatic or asymptomatic in regardless of Anemia. The most reported symptoms are dizziness, fatigue, low concentration, headache, tinnitus and dizziness. In some vulnerable patients, restless leg syndrome can also be seen.
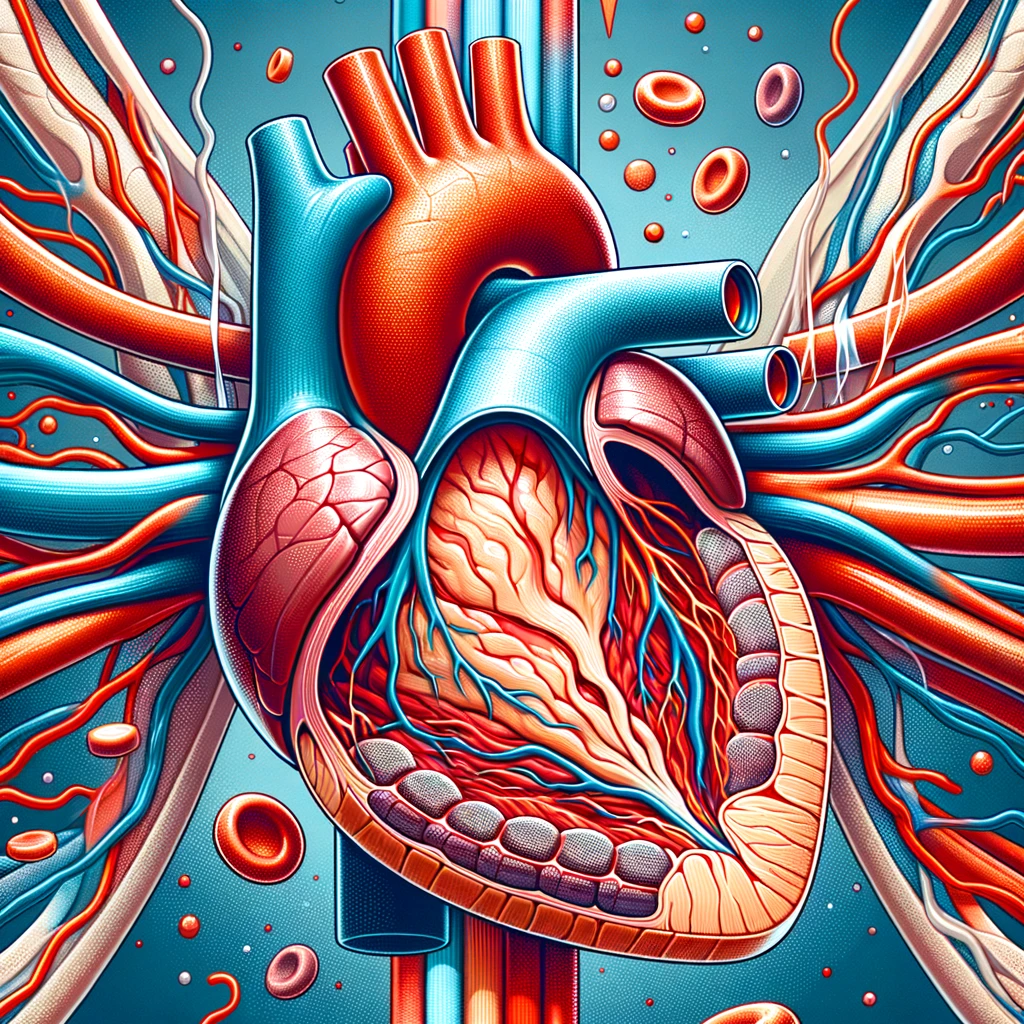
Iron deficiency and Anemia may deteriorate some diseases’ symptoms as well, which are heart failure and ischemic heart diseases. In severe cases, hemodynamic instability might even occur.
Daily recommended of iron intake is as the following,
· 11 mg for infants between 7- and 12-month-olds.
· 18 mg for women in pre-menopause,
· 27 mg for pregnant women,
· 8 mg for adult men.
Iron in meat is found as Hem, whereas it is found as non-Hem in vegetation. The form of Hem-Iron is absorbed effectively and its absorption is not affected by other factors, while the non-Hem form is poorly absorbed and may undergo interactions with other nutrients. To give an example, Vitamin C enhances the absorption of non-Hem iron however, tannins which are found in tea and coffee inhibit the absorption of non-Hem. The iron absorbed from a vegetation diet is less effective than the one absorbed from meat. Therefore, iron deposits are lower in vegetarian people which makes them vulnerable to iron deficiency.
The use of Iron Supplements
First of all, the reason underlying the condition must be determined. For instance, eradication of H.pylori infection and introduction of food containing Gluten to celiac disease affects the absorption of iron. Undertaking efforts not only prevents the further iron loss but also enhances the absorption of iron.
The main question in the iron deficiency treatment is whether it should be done orally or IV. The right treatment is chosen depending on the patients’ age, sex, the severity of the cause of deficiency and other symptoms.
IV treatment is usually begun when there is no response to oral treatment with severe Anemia or when the oral treatment is not tolerated or has low adherence. Oral treatment can be started as long as it is not contraindicated, and patients’ conditions determine treatment duration and monitoring. If not tolerated or tolerance develops, other formulations could be used or H. pylori infection could be eradicated or gluten-free diet could be introduced to patients with celiac disease, even if all these measurements are not useful, IV treatment could be considered.
The table given below summarizes the differences between oral and IV treatment.
| Parameters | Oral | IV |
| Absorption and Bioavailibility | Iron absorption is low when given orally. Absorption decreases in cases of infection |
Absorption is not affected by inflammation |
| Administration Ease | Easy | Administration site reactions and hypersensitivity reactions that can be fatal could be developed |
| Dosing | It can be given up to three times daily | It can be given either single dose or multiple doses |
| Response | Response for oral treatment is limited | The treatment is effective and levels of iron increase in a short time |
| GI adverse effects | The probability of GI side effects is high | GI side effects are usually not observed |
| Other side effects | Skin discoloration may develop | Headache, Hypophosphatemia and in some formulations osteomalaceia may occur |
| Adherence | Low | High |
| Cost | Low | High |
References:
Cappellini, M. D., Musallam, K. M., & Taher, A. T. (2019). Iron deficiency anaemia revisited. In Journal of Internal Medicine (Vol. 287, Issue 2, pp. 153–170). Wiley. https://doi.org/10.1111/joim.13004
Clara Camaschella; Iron deficiency. Blood 2019; 133 (1): 30–39. doi: https://doi.org/10.1182/blood-2018-05-815944
Pasricha, S.-R., Tye-Din, J., Muckenthaler, M. U., & Swinkels, D. W. (2021). Iron deficiency. In The Lancet (Vol. 397, Issue 10270, pp. 233–248). Elsevier BV. https://doi.org/10.1016/s0140-6736(20)32594-0
In the ever-evolving landscape of healthcare, the discipline of pharmacoeconomics has emerged as a vital tool for maximizing the value of healthcare resources and optimizing patient outcomes.
Myocardial infarction or acute myocardial infarction are the other terms for heart attack. The heart attack occurs when the blood supply to some certain areas to heart is disrupted and the heart muscle lacks oxygen and therefore gets damaged. In coronary arteries, which supply the heart, sometimes an obstruction may also occur. What this means is that an unstable plaque that consists of fat, cholesterol and white blood cells is formed and obstruct the vessel.
In the realm of healthcare, effective communication is paramount, especially when it comes to ensuring therapeutic safety for patients.
Once the Vitamin B12 is absorbed, it plays a key role as a cofactor in the synthesis of DNA, fatty acids or myelin. Therefore, Vitamin B12 deficiency could lead to both hematologic and neurologic symptoms.