In the realm of healthcare, effective communication is paramount, especially when it comes to ensuring therapeutic safety for patients. The collaboration and coordination between physicians play a crucial role in preventing medical errors, optimizing treatment outcomes, and ultimately safeguarding patient well-being. In this blog post, we’ll explore the importance of communication between physicians in promoting therapeutic safety and enhancing the quality of patient care.
One of the primary reasons why communication between physicians is essential for therapeutic safety is the complexity of modern healthcare. Patients often receive care from multiple healthcare providers across different specialties and settings, such as primary care physicians, specialists, surgeons, and hospitalists. Each physician brings unique expertise and perspectives to the table, but without effective communication channels, there is a risk of fragmented care and miscommunication.
Effective communication between physicians ensures that crucial information about a patient’s medical history, current condition, treatment plan, and medication regimen is accurately conveyed and understood by all members of the healthcare team. This helps prevent misunderstandings, duplication of tests or treatments, and potential conflicts or contradictions in care recommendations. By fostering a shared understanding of the patient’s care needs and goals, communication between physicians facilitates collaborative decision-making and promotes continuity of care across transitions in care settings.
Moreover, communication between physicians is essential for coordinating care and managing complex medical cases effectively. In situations where a patient’s care involves multiple specialists or interdisciplinary teams, clear and timely communication is vital for ensuring that all aspects of the patient’s treatment plan are integrated and coordinated seamlessly. This includes sharing relevant diagnostic findings, treatment updates, and follow-up recommendations to ensure that care is delivered in a cohesive and patient-centered manner.
Additionally, communication between physicians is critical for identifying and mitigating potential risks to patient safety. Healthcare providers must be able to communicate openly and transparently about adverse events, near misses, or concerns regarding patient care. By fostering a culture of safety and collaboration, physicians can work together to identify system weaknesses, implement corrective actions, and prevent similar incidents from occurring in the future.
Furthermore, effective communication between physicians can enhance patient satisfaction and engagement in their care. When patients perceive that their healthcare providers are communicating effectively and working collaboratively on their behalf, they are more likely to feel informed, supported, and empowered to participate actively in their treatment decisions. This, in turn, can lead to better treatment adherence, improved health outcomes, and greater overall satisfaction with the healthcare experience.
In conclusion, communication between physicians is a cornerstone of therapeutic safety in healthcare. By facilitating collaboration, coordination, and information sharing among members of the healthcare team, effective communication ensures that patients receive high-quality, coordinated care that is tailored to their individual needs and preferences. Healthcare organizations must prioritize communication skills training, utilize technology-enabled communication tools, and foster a culture of teamwork and mutual respect to promote therapeutic safety and enhance patient outcomes. Ultimately, investing in effective communication between physicians is an investment in the safety, quality, and integrity of patient care.
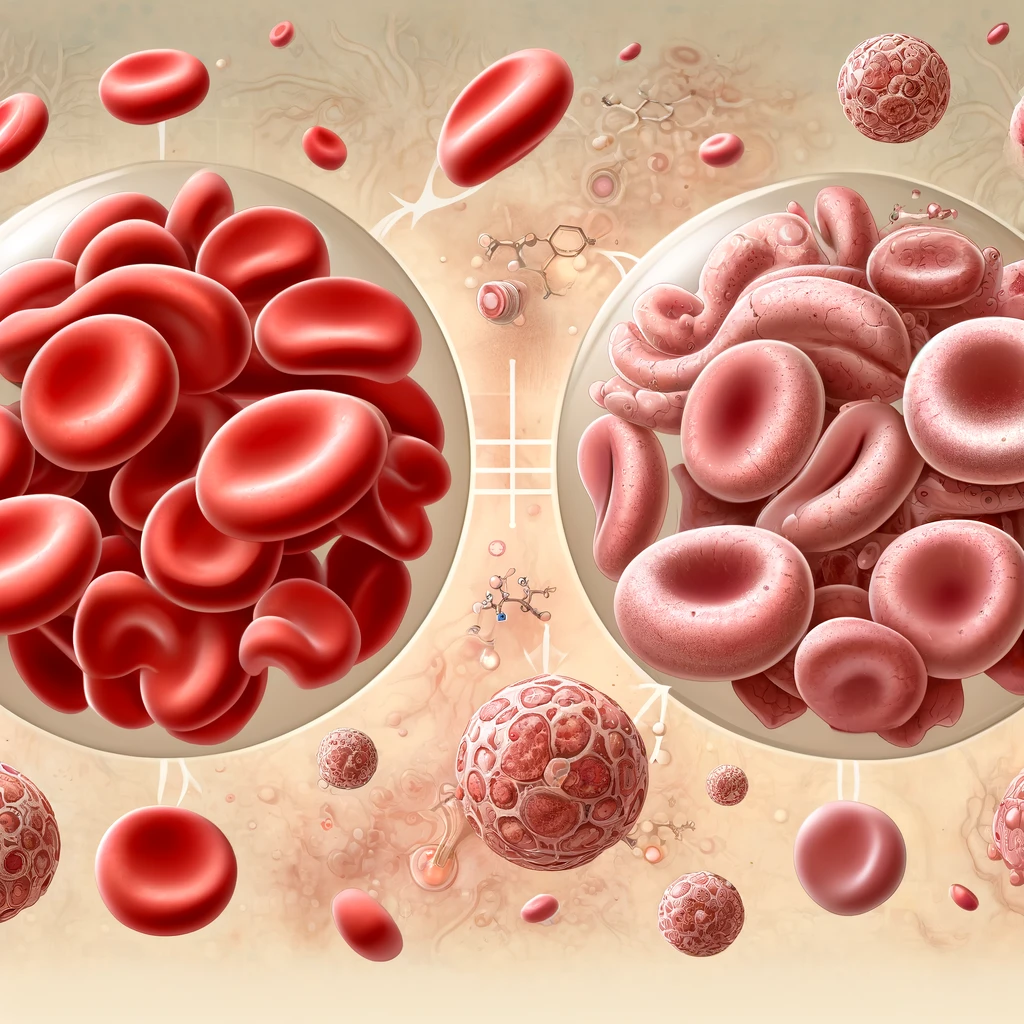
Iron Deficiency and Iron Deficiency related anemia contributes to several diseases worldwide. In 2016, more than 1.2 billion cases of iron deficiency anemia were reported. Iron deficiency anemia affects children, women in pre-menopause and people in low and middle income countries more.
In the ever-evolving landscape of healthcare, the discipline of pharmacoeconomics has emerged as a vital tool for maximizing the value of healthcare resources and optimizing patient outcomes.
Myocardial infarction or acute myocardial infarction are the other terms for heart attack. The heart attack occurs when the blood supply to some certain areas to heart is disrupted and the heart muscle lacks oxygen and therefore gets damaged. In coronary arteries, which supply the heart, sometimes an obstruction may also occur. What this means is that an unstable plaque that consists of fat, cholesterol and white blood cells is formed and obstruct the vessel.
Once the Vitamin B12 is absorbed, it plays a key role as a cofactor in the synthesis of DNA, fatty acids or myelin. Therefore, Vitamin B12 deficiency could lead to both hematologic and neurologic symptoms.